Development of an Impedance Based Screening Assay for Cardiac Safety and Cardiotoxicity Detection in Stem Cell-derived Cardiomyocytes
Case Study
Case Study title
Development of an Impedance Based Screening Assay for Cardiac Safety and Cardiotoxicity Detection in Stem Cell-derived Cardiomyocytes
Authors
Robert W. Kirby, Said El Haou, Edward Humphries, John Ridley and Marc Rogers
- Metrion Biosciences Ltd, Riverside 3; Suite 1, Granta Park, Cambridge, CB21 6AD, United Kingdom
Introduction
Cardiac toxicity remains the leading cause of new drug safety side-effects. Current preclinical cardiac safety assays rely on in vitro cell-based ion channel assays and ex vivo and in vivo animal models⁽¹⁾. These assays provide an indication of acute risk but they do not always predict the effect of chronic compound exposure, as recently seen with oncology drugs⁽²⁾. Therefore, new assays are required to characterise chronic structural and functional effects in human cells earlier in drug discovery⁽²̛ ³⁾. Impedance-based technology can provide more accurate chronic cardiotoxicity measurements in an efficient manner using human induced pluripotent stem cell-derived cardiomyocytes (hiPSC-CMs)⁽¹̛ ³⁾.
Here we outline validation of chronic cardiotoxicity assays using an impedance platform in combination with commercial hiPSC-CMs:
- Impedance readouts can be reliably measured and are stable to allow acute (< 24 hrs) as well as longer duration (72 hrs) testing.
- Identify the acute and chronic effects of clinical cardiac ion channel modulators against cardiomyocyte contractility and viability.
- Confirm that structural and functional cardiotoxicity of clinical compounds arising from multiple cellular and signalling mechanisms could be detected in an acute and/or chronic assay timeframe.
Materials and methods
hiPSC-CMs from commercial vendors (Ncardia and CDI) were plated onto CardioExcyte96 well plates (Nanion) according to manufacturers’ instructions. Plates were incubated at 37 °C (5 % CO2 ) for 7-10 days and 100 % medium exchanges were performed daily. Impedance signals were recorded using the CardioExcyte96 (CE96) platform and the formation of a spontaneous beating syncytial network was monitored with 30 s impedance recording every hour (1 hr) during the first week in culture.
A single concentration of compound was then applied to each well (N ≥ 4) every 24 hrs as a 1:1000 fold dilution into media (final = 0.1 %) for a maximum of 72 hours before a washout period. The outputs (Figure 1) were recorded at 60 minute intervals to assess acute vs. chronic effects (< 24 hrs vs 24 – 72 hrs).
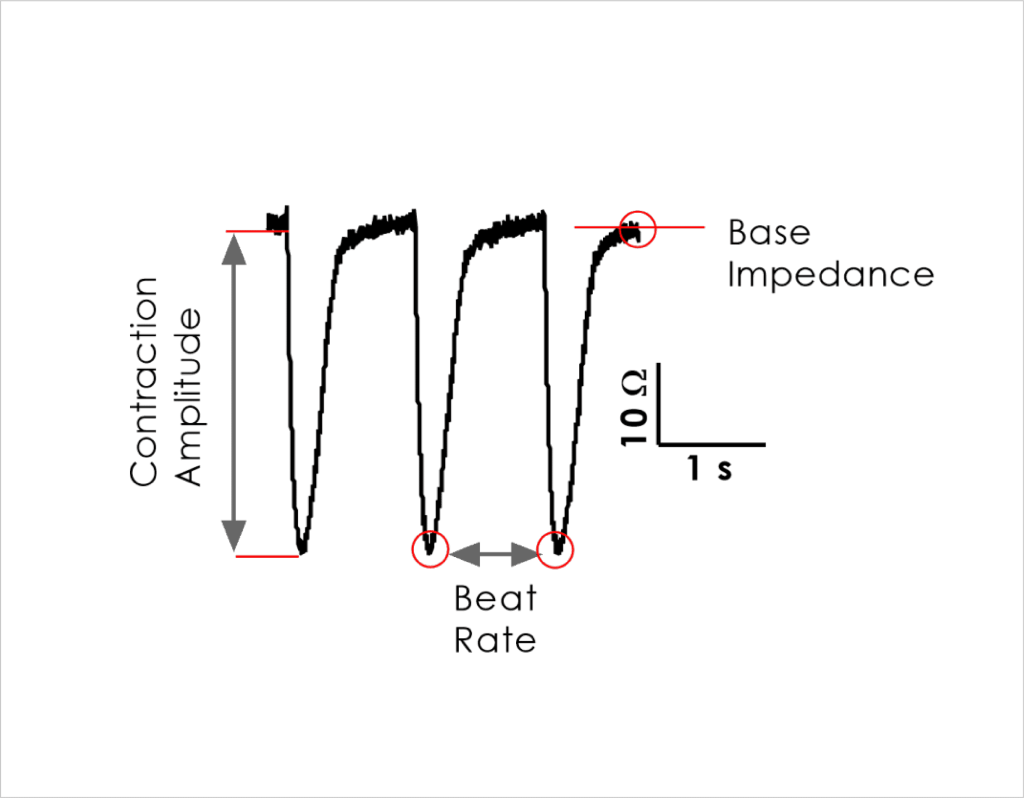
Impedance assay
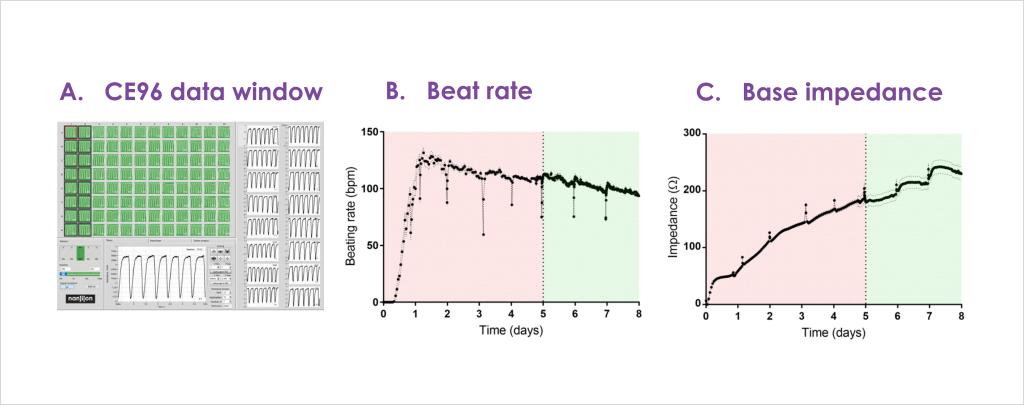
hiPSC-CMs from a commercial vendor plated onto a CardioExyte96 well plate delivered a high success rate across the plate
(A) Greater than 90% of wells started beating within 6 hours and stabilised within 72 hours
(B) Consistent base impedance (growth phase) parameters were obtained after 5 days
(C) Recordings were suitable for chronic drug screening after 4-7 days
Cardiac ion channel modulator effects on contractility
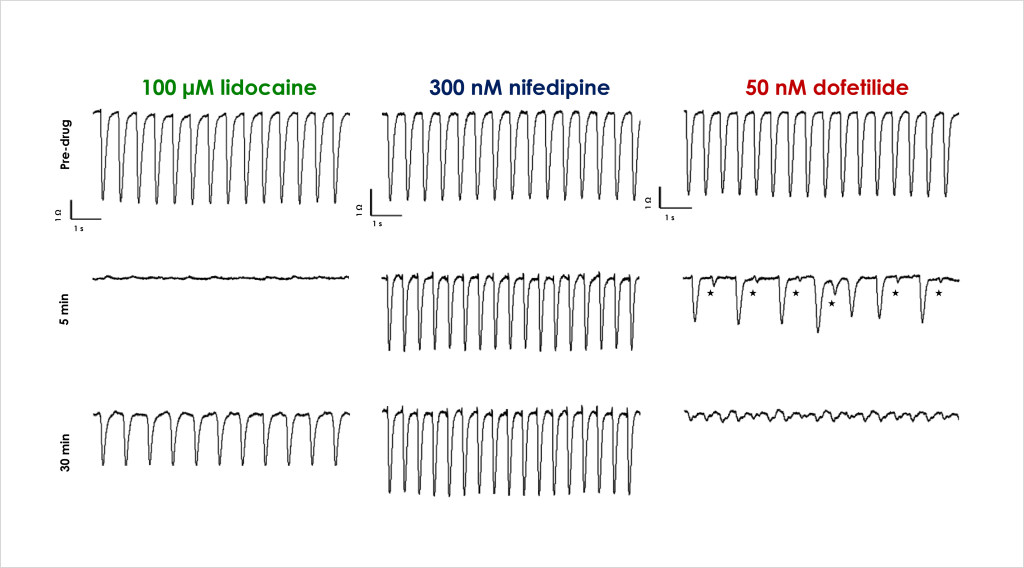
A. Acute effects of ion channel ligands on cell contraction
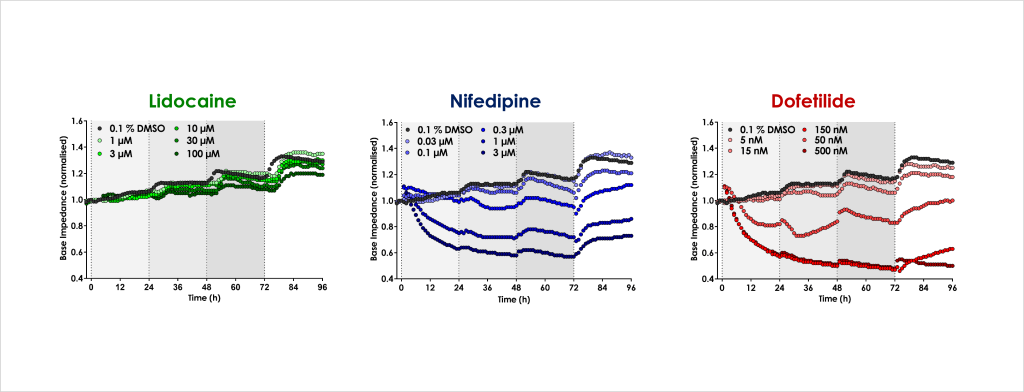
B. Chronic cardiotoxicity drug effects
(A): Cardiac contractility was assessed by examining changes in beat rate and amplitude. The expected acute effects of cardiac ion channel modulators of IKr (dofetilide, 50 nM), INa (lidocaine, 100 µM) and ICa (nifedipine, 300 nM) were confirmed, as represented by the traces above showing spontaneous contractile activity in control conditions (Pre-drug) and in presence of drug after 5 and 30 min incubation. Lidocaine stopped contraction but beating recovered with a decreased beat rate & amplitude, nifedipine increased beat rate but decreased amplitude, and dofetilide decreased amplitude & beat rate with secondary beats degenerating into fibrillation.
(B): Chronic cardiac drug effects on base impedance Base impedance was used to monitor cell viability over 72 hour period. Lidocaine had no effect at 72 hrs relative to control whereas nifedipine and dofetilide produced time- and concentration-dependent decreases in base impedance within 24 hrs.
Chronic cardiotoxicity mechanisms
Functional and structural cardiotoxic effect of drugs with different modes of action, including several therapeutic oncology reagents, were tested. Drug mechanisms included DNA intercalation (doxorubicin), proteasome inhibition (bortezomib), myosin disruption (blebbistatin), SERCA Ca2+ pump inhibition (thapsigargin), kinase inhibition (Sunitinib), and an ion channel modulator with mixed functional and structural effects (amiodarone). Aspirin is considered non-cardiotoxic and was used as a negative control⁽⁴⁾.
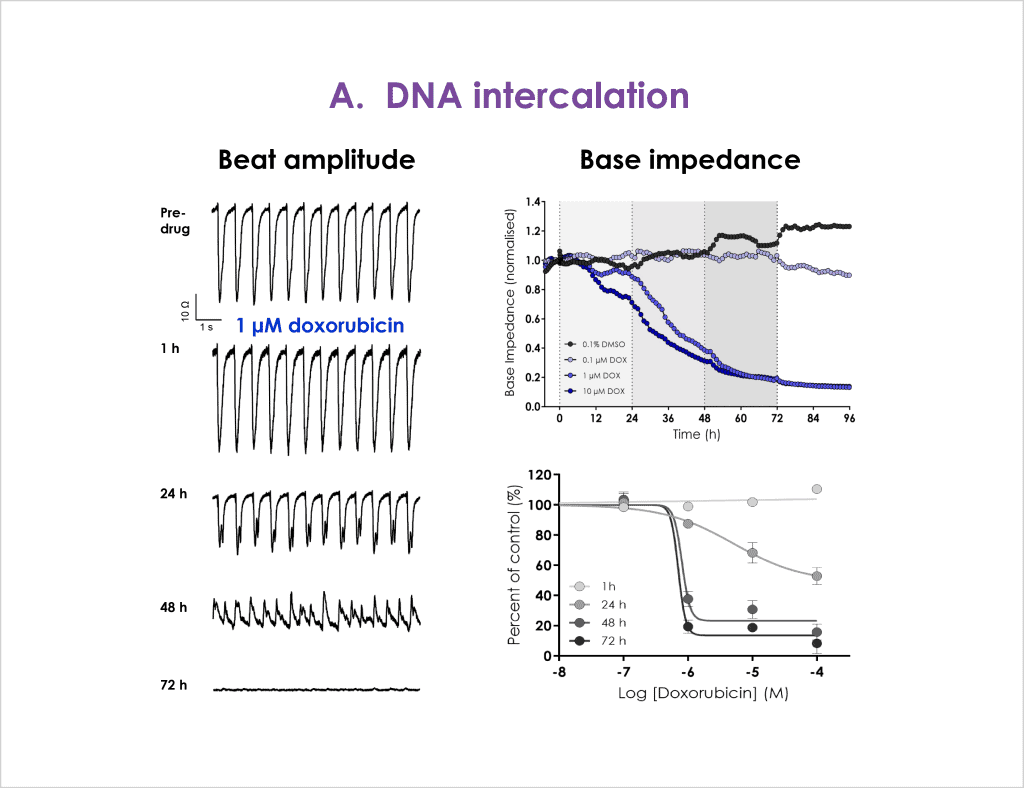
A. DNA intercalator
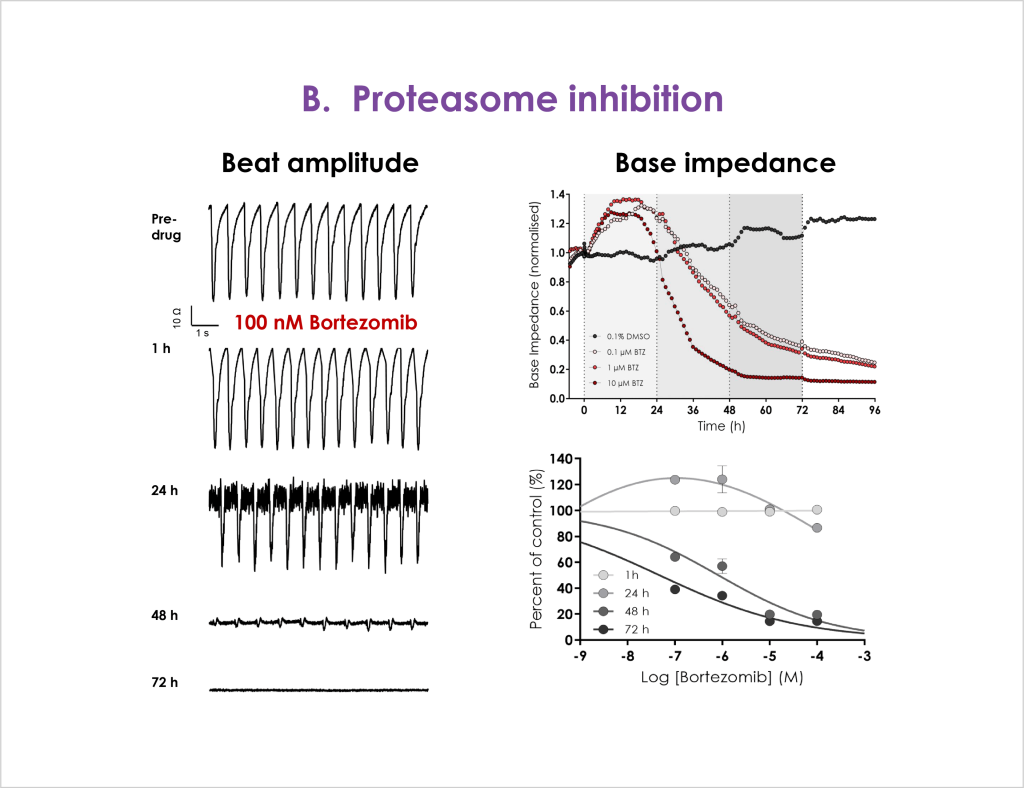
B. Proteosome inhibitor
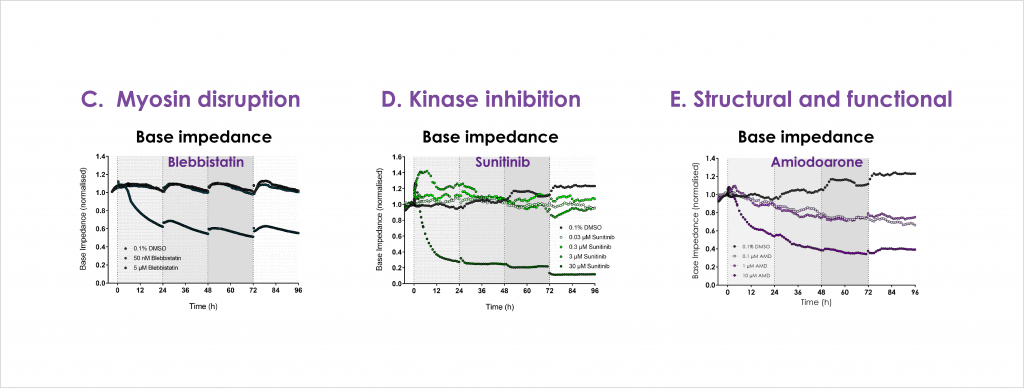
C. Myosin disruptor, D. Kinase inhibitor and E. Structural and functional inhibitor
F. SERCA Ca2+ pump inhibitor and G. Negative control
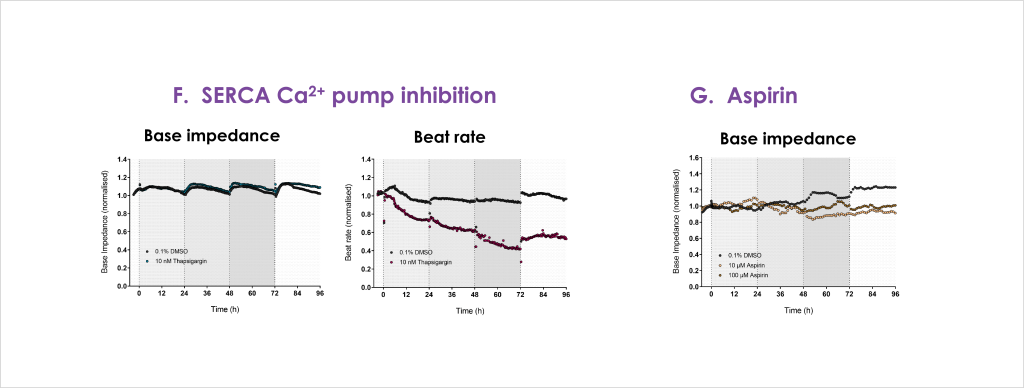
Concentration and time-dependent decreases in base impedance were observed for doxorubicin with > 24 hrs required to resolve the full effect (A). Bortezomib produced biphasic effects, initially increasing base impedance (< 24 hrs) at all concentrations tested, before impairment of contractility was seen at > 24 hrs (B). The myosin disruptor blebbistatin produced a rapid and sustained reduction in base impedance within 24 hrs (C). Similar to bortezomib, the oncology kinase inhibitor sunitinib produced a transient and dose-dependent increase in base impedance at 3 and 30 µM before longer incubation and higher concentrations disrupted base impedance (D). The non-specific ion channel modulator amiodarone also produced concentration and time-dependent deficits in cell impedance (E). The Ca2+ pump inhibitor thapsigargin showed a small tendency to increase base impedance, and as expected more pronounced effects on beat rate contractility due to depletion of intracellular calcium stores (F). The negative control Aspirin showed little concentration or time-dependent effects on cell impedance (G).
H. Atypical cardiac toxicity of Trastuzumab
Trastuzumab is a monoclonal antibody approved for treating HER2-positive breast and gastric cancer. However, clinical incidents and post-market analysis reveal that therapeutic use has been limited by the occurrence of adverse cardiac events, the mechanism(s) of which are not fully realised⁽⁵⁾.
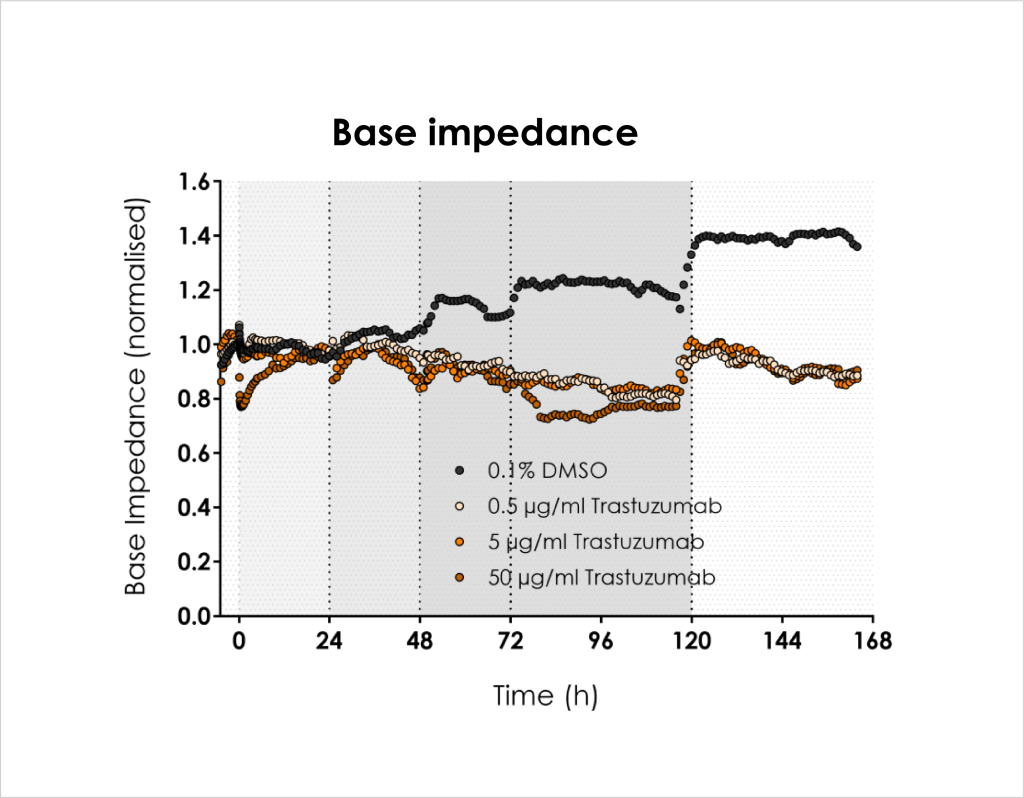
Figure 5: Trastuzumab (0.5 – 50 µg/ml) was applied at 0, 24, 48 and 72 hrs after base impedance stability was achieved. Significant effects on base impedance relative to control were only recorded > 72 hrs following multiple applications of antibody, suggesting either that entry into the cell is limited or the modulation of substrates responsible for this cardiotoxicity is slowacting.
Conclusions
- The combination of CE96 impedance platform and commercial human stem cell-derived cardiomyocytes delivers a stable and consistent assay with a high success rate across every 96 well plate, enabling the reliable screening of acute and chronic cardiotoxicity effects of test compounds.
- Surprisingly, we detected chronic functional and structural effects of known cardiac ion channel modulators, in addition to their expected acute effects on cell excitability and contraction.
- This assay platform can reliably detect the chronic cardiotoxicity effects of clinical compounds with diverse mechanisms-of-action, indicating its utility as part of a translational cardiac safety testing regime.
Acknowledgements
Authors would like to thank former Metrion cell culture manager Louise Webdale and Metrion summer intern student Luka Smalinskaite for their assistance with the experiments.
References
- Ferdinandy et al., (2019). European Heart Journal. PMID: 29982507
- Scott et al., (2014). Toxicological Sciences. PMID: 23237062
- Koci et al., (2017). Toxicology and Applied Pharmacology. PMID: 28546047
- Clements et al., (2015). Toxicological Sciences. PMID: 26259608
- Mohan et al., (2018). Antibody Therapeutics. PMID: 30215054

Let’s work together
What are your specific ion channel and assay needs?
If you have any questions or would like to discuss your specific assay requirements, we will put you directly in touch with a member of our scientific team. Contact us today to discover more.